What Causes Depression? Understanding the Underlying Issues | GrandRising Behavioral Health
Explore the underlying causes of depression and how it affects daily life. Learn about the roots of this challenging mental health condition.

Depression is a complex mood disorder marked by persistent low mood, loss of interest, and changes in sleep, appetite, or concentration. [1] Understanding what causes depression guides more effective care and recovery.
This page outlines the most common drivers, biological, psychological, and environmental, and explains how genes, brain chemistry, trauma, and life stressors interact to produce symptoms.
You’ll find clear explanations of biological mechanisms (like neurotransmitters and hormones), psychological contributors (including adverse childhood experiences and unhelpful thought patterns), and social triggers such as grief, isolation, and substance use.
We also include practical signs for when to seek help and the evidence-based treatments typically used in outpatient care.
What Are the Main Biological Causes of Depression?
Biological contributors include inherited risk, changes in brain chemistry and neural circuits, and medical or hormonal conditions that affect mood regulation. [2]
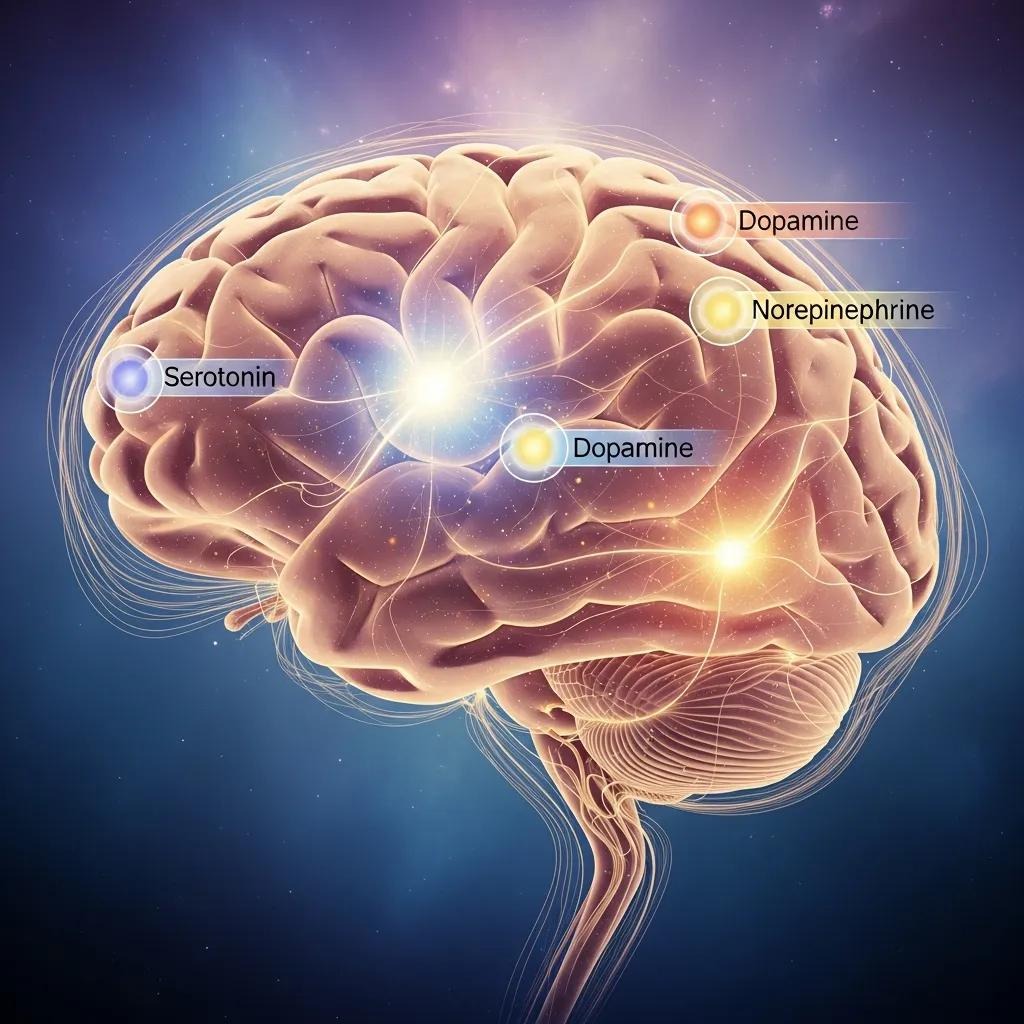
A family history raises baseline risk, but genes interact with life experiences, so heredity is a risk factor, not a destiny. Imbalances in neurotransmitters such as serotonin, norepinephrine, and dopamine, and altered communication between brain regions that regulate emotion, are linked to symptoms like loss of pleasure and slowed thinking. [3]
Medical issues, such as thyroid problems, menopause-related hormone changes, side effects of certain medications, or chronic illness, can also trigger depressive episodes. [4] Because of this, a medical assessment is often an important first step in care, alongside psychiatric treatment.
The comparison below shows how different biological contributors affect risk and shape treatment targets.
This comparison helps explain why some people benefit from medical evaluations or medication while others respond more to psychotherapy. Keep biological vulnerability in mind as you read about psychological contributors and stress responses.
Practical biological steps:
- Start with a medical history and basic lab tests to rule out underlying causes of mood change.
- Medication management helps address neurotransmitter imbalances and is often combined with psychotherapy for better results.
- Treating underlying medical or hormonal issues may significantly reduce depressive symptoms.
These steps highlight the value of coordinated medical and psychiatric assessment and lead into psychological causes that interact with biology.
How Genetic Predisposition Can Increase Depression Risk
Genetic predisposition raises the likelihood of developing major depressive disorder, but doesn’t determine the outcome on its own. Research shows a moderate heritable component: having relatives with depression increases risk, yet many people with a family history never develop the disorder. [5]
Gene–environment models explain how life stress, trauma, or chronic illness can trigger symptoms in those with genetic vulnerability. Knowing a person’s family history helps clinicians tailor monitoring, consider early interventions, and discuss strategies to reduce future risk.
What Role Do Brain Chemistry and Neurotransmitters Play in Depression?
Neurotransmitters shape mood, motivation, and reward; imbalances in serotonin, norepinephrine, and dopamine are linked to core depressive symptoms such as low mood, loss of pleasure, and low energy. [6]
Dysfunctional circuits, notably between prefrontal control areas and limbic emotion centers, can produce persistent negative mood and poor stress regulation. These circuit changes may be both a cause and a consequence of chronic depression.
Medications aim to rebalance neurotransmitters, while psychotherapy supports neural plasticity through changes in behavior and thought. Evidence shows that combining medication with psychotherapy often improves the chances of remission.
How Do Psychological Factors Contribute to Depression?
Psychological contributors include trauma and adverse childhood experiences (ACEs), certain personality traits, and habitual thinking patterns such as rumination and negative bias that keep mood low. Early trauma can sensitize the stress-response system and disrupt attachment and emotion regulation, increasing lifetime vulnerability to depression. [7]
Traits like high neuroticism and limited coping skills raise the risk of prolonged or recurrent episodes. Cognitive habits, for example, catastrophizing or learned helplessness, maintain depressive thinking and reduce engagement with life. Evidence-based therapies that target these processes can reduce symptoms and lower long-term risk.
The comparison below illustrates how psychological factors differ in mechanism and outcome.
This comparison explains why trauma-informed care and cognitive interventions are central to treatment planning. Common evidence-based therapies used in outpatient settings include:
- Trauma-focused approaches such as EMDR and trauma-informed CBT help process and integrate traumatic memories.
- Cognitive therapies like CBT target unhelpful thinking and rumination to reduce symptom persistence.
- Skills-based treatments such as DBT teach emotion-regulation and distress-tolerance strategies for intense mood states.
These therapeutic options are widely offered in outpatient clinics and lead to a discussion of environmental triggers that often precipitate episodes.
How Trauma and Adverse Childhood Experiences Can Lead to Depression
Yes. ACEs and repeated early stress significantly increase risk for adult depression by altering stress physiology, attachment, and emotion regulation. Early adversity can sensitize the HPA axis and shift neural development toward heightened threat detection, making depressive responses more likely under later stress. [8]
Trauma-related depression often co-occurs with PTSD and benefits from trauma-informed assessment and targeted treatments such as adapted CBT or EMDR. [9] Identifying trauma histories allows clinicians to select therapies that reduce reactivity and restore functioning.
This focus on trauma connects to personality and cognitive patterns that help sustain depressive episodes.
How Personality Traits and Thinking Patterns Affect Depression
Personality features like high neuroticism and persistent cognitive styles such as rumination and catastrophizing both increase vulnerability to depression and help maintain symptoms.
Rumination extends negative mood by repeatedly focusing on problems without problem-solving, while avoidant coping reduces engagement with rewarding activities. Interventions that change these patterns, behavioral activation, cognitive restructuring, and targeted skills training, decrease symptom severity and lower relapse risk.
Early identification of maladaptive cognitive styles enables focused psychotherapy to build resilience and healthier coping.
With psychological drivers in mind, we turn to social and environmental triggers that often precipitate first episodes.
What Environmental and Social Triggers Cause Depression?
External triggers include acute losses, chronic stressors, social isolation, economic hardship, workplace strain, and substance use. These factors interact with biological vulnerability and psychological patterns to determine when and how depression appears. Social determinants such as poverty and discrimination raise risk across populations. [10]
Interventions that strengthen social support, reduce substance-related harm, and address practical stressors can meaningfully change the course of depression. Recognizing modifiable triggers helps clinicians and patients target interventions through community, clinical, and medical pathways.
The table highlights how external factors differ and where social or clinical interventions can be applied. Community and program supports that often help include:
- Group therapy and community programs reduce isolation and strengthen coping resources.
- Integrated outpatient addiction care addresses co-occurring substance use and mood symptoms.
- Outpatient programs that emphasize peer support and connection can lower relapse risk and improve daily functioning.
How Do Stressful Life Events and Social Isolation Trigger Depression?
Acute losses and ongoing stress can activate grief, helplessness, and prolonged stress-response engagement, shifting mood and thinking toward depression. Social isolation removes important emotional buffering and compounds risk.
While bereavement often causes temporary sadness, persistent stressors or lack of support can lead to clinical depression with functional decline. Practical steps, rebuilding social ties, structured problem-solving, and seeking professional help early, can prevent situational distress from evolving into a depressive disorder.
Timely engagement with supportive resources is protective and can alter the course of distress. This leads to substance use, a common co-occurring issue that often complicates recovery.
The Link Between Substance Use and Depression
Substance use and depression influence each other bidirectionally: people may use substances to self-medicate, but substances also change brain chemistry and stress systems in ways that worsen mood and increase relapse risk.
Alcohol and sedatives can deepen low mood and disrupt sleep; stimulants may cause crash-related depression. [11] Withdrawal states can mimic or trigger depressive episodes. Integrated treatment that addresses both mood and substance use together produces better outcomes than treating either condition alone.
Early recognition of comorbidity enables coordinated care that reduces substance-related harm and improves mood. This evidence sets the stage for understanding stress physiology and when to seek professional assessment.
How Are Stress and Depression Connected?
Stress and depression are linked by physiological pathways (such as HPA axis dysregulation and elevated cortisol) and psychological mechanisms like learned helplessness and chronic worry that keep depressive states active. Long-term stress changes brain structure and function in areas that govern mood and decision-making, which can sustain symptoms even after the original stressor ends.
Effective care often combines stress-focused strategies, sleep improvement, behavioral activation, skills training, with medical evaluation when hormonal or inflammatory contributors are suspected. Understanding how stress affects mood helps clarify when self-care is enough and when professional help is needed.
How Stress Hormones Can Affect Depression
Chronic elevation of cortisol and HPA axis dysregulation can disrupt sleep and appetite and impair neural plasticity, contributing to persistent low mood and cognitive difficulties seen in depression.
Long-term cortisol exposure may reduce hippocampal volume and alter amygdala responsiveness, which undermines memory and emotion regulation and increases sensitivity to later stress.
These hormonal effects also interact with neurotransmitter systems, sometimes making symptoms harder to treat without targeted interventions. Recognizing stress-related biological changes helps clinicians choose combined medical and psychotherapeutic strategies to restore balance and function.
This biological context leads to a practical checklist for when to seek professional help.
When to Seek Help for Stress-Related Depression
Seek professional evaluation if depressive symptoms persist for two or more weeks with noticeable decline in daily functioning, if you have suicidal thoughts, or if substance use, severe sleep loss, or medical problems are worsening your mood. Immediate attention is required for any thoughts of self-harm, significant withdrawal from normal activities, or inability to meet basic needs.
Grand Rising Behavioral Health offers evidence-based outpatient options for depression treatment in Massachusetts, including Intensive Outpatient (IOP) and standard Outpatient (OP) programs, with in-person and premium virtual care, group and individual therapy, and medication management.
If you meet these thresholds, contact our clinical intake team to discuss the most appropriate coordinated care.
Help-seeking checklist:
- Duration: Depressed mood or loss of interest lasting 2+ weeks with daily impact.
- Function: Notable decline at work, school, or in relationships.
- Safety: Any suicidal thoughts, plans, or self-harm behaviors.
When these criteria apply, coordinated clinical assessment and treatment offer the best path toward recovery.
Frequently Asked Questions
What Are the Early Warning Signs of Depression?
Early signs include ongoing sadness or loss of interest in activities you used to enjoy, changes in sleep or appetite, trouble concentrating, low energy, and feelings of worthlessness or excessive guilt. Physical symptoms such as persistent fatigue or aches without a clear medical cause can also appear.
Noticing these signs early makes it easier to get help and improve outcomes. If you or someone you know shows these symptoms, reach out to a mental health professional or your primary care provider.
How Can Lifestyle Changes Help Manage Depression?
Lifestyle changes can support recovery and reduce symptoms. Regular movement, balanced nutrition, and consistent sleep build resilience. Staying socially connected, maintaining routines, and practicing mindfulness or relaxation techniques can reduce stress and lift mood.
While these lifestyle steps help, they often work best alongside therapy or medication when symptoms are moderate to severe.
What Types of Therapy Are Effective for Treating Depression?
Several therapies have strong evidence for treating depression. Cognitive Behavioral Therapy (CBT) addresses negative thought patterns and behaviors. Interpersonal Therapy (IPT) focuses on relationship and role-related issues.
Dialectical Behavior Therapy (DBT) teaches emotion-regulation skills for intense mood swings. Trauma-focused approaches like EMDR help process traumatic memories that may drive symptoms. The best choice depends on individual needs and clinical assessment.
How Does Social Support Impact Recovery from Depression?
Social support is a powerful protective factor. Trusted friends, family, or support groups provide emotional comfort, reduce isolation, and encourage treatment engagement. People with solid social connections often recover faster and have lower relapse rates. Building and sustaining meaningful relationships is an important part of recovery planning.
Disclaimer
The information in this article is meant for educational and informational purposes only. It should not replace professional medical or mental-health advice, diagnosis, or treatment. Grand Rising Behavioral Health offers evidence-based outpatient programs (including PHP, IOP, and OP), but individual needs and treatment timelines may vary.
If you or a loved one is dealing with mental health concerns, please reach out to Grand Rising Behavioral Health’s admissions team for a confidential consultation. Our licensed clinicians can evaluate your needs and help you start a safe, personalized care plan without delay.
Reference
1. https://www.nimh.nih.gov/health/publications/depression
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC2950973/
3. https://www.mentalhealth.com/library/biology-of-depression-neurotransmitters
4. https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
5. https://med.stanford.edu/depressiongenetics/mddandgenes.html
6. https://www.mentalhealth.com/library/biology-of-depression-neurotransmitters
7. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2022.748372/full
8. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2022.748372/full
9. https://www.ptsd.va.gov/understand/related/depression_trauma.asp
10. https://www.who.int/news-room/fact-sheets/detail/depression
11. https://www.helpguide.org/mental-health/addiction/self-medicating
More Resources
A team ready to start your journey.
Get in touch — today.
We are a safe space – a haven for exceptional individuals to receive discreet, personalized, in-person treatment and care.
.avif)










