What Are the Causes of Major Depressive Disorder? | GrandRising Behavioral Health
Learn about the causes of Major Depressive Disorder and how it can affect daily life. Get clear information to support effective mental health care and treatment decisions.

Major Depressive Disorder (MDD) is a disabling mood disorder marked by persistent low mood, loss of interest in usual activities, and reduced daily functioning. [1] Its origins are rarely due to a single factor; biological, psychological, and environmental contributors typically combine to produce symptoms. [2]
Recognizing these root causes helps explain why some people have isolated episodes while others experience recurrence, and guides more precise treatment choices, from psychotherapy and medication to different levels of outpatient care.
This article reviews the main biological mechanisms (genes, neurotransmitters, hormones, inflammation), psychological processes (rumination, cognitive distortions, personality traits), and environmental triggers (adverse childhood experiences, bereavement, chronic stress) that raise risk for MDD.
This page provides clear explanations of how each domain works, concise cause→treatment mappings, and practical information about evidence-based outpatient options for adults in Massachusetts.
What Are the Main Biological Factors in Major Depressive Disorder?
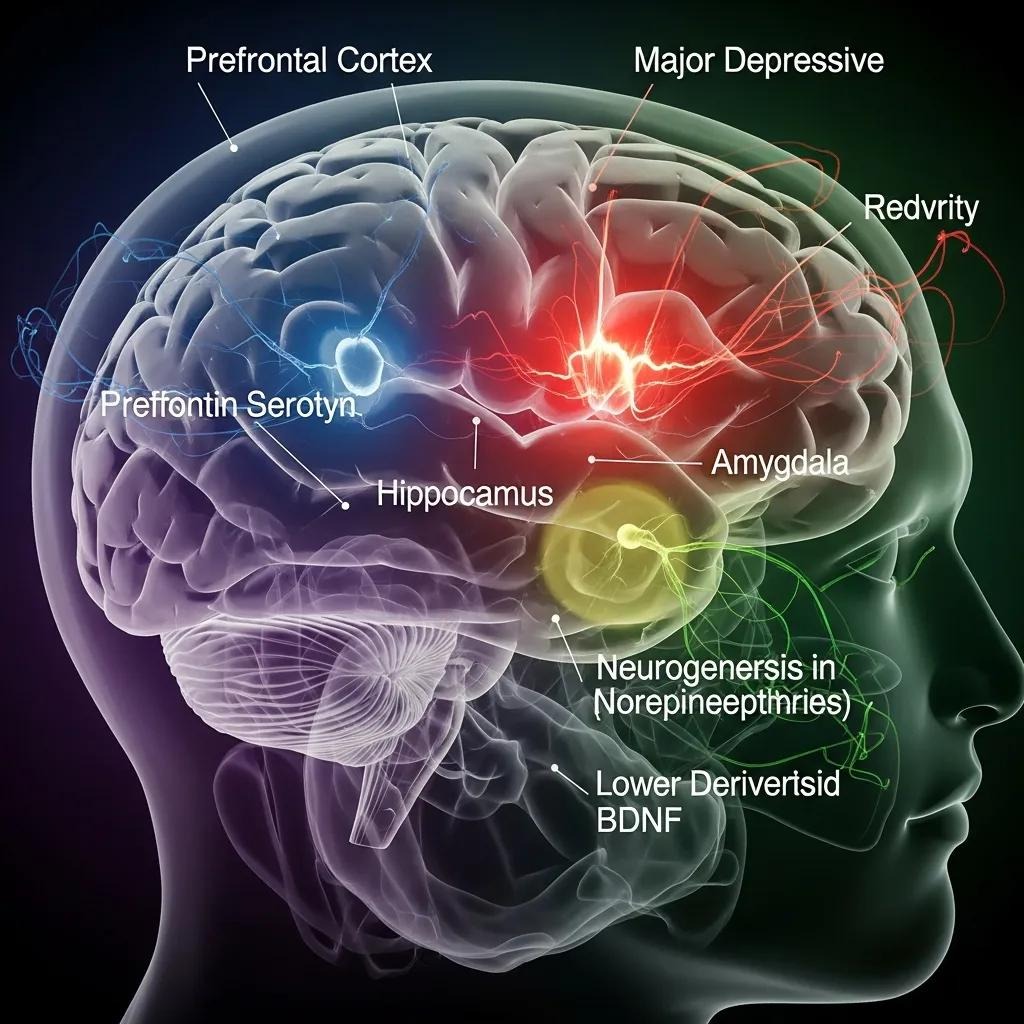
Biological contributors include inherited vulnerability, differences in neurotransmitter systems, dysregulation of hormones and the HPA axis, structural and functional brain changes, and inflammatory processes that influence mood regulation.
Together, these factors alter neural circuits for reward, motivation, and stress response and can produce symptoms such as anhedonia, low energy, and slowed thinking. Contemporary research treats these as interacting risks, not a single “chemical imbalance”, highlighting gene–environment interactions and the long-term effects of stress on the body and brain.
In clinical practice, providers weigh biological markers and medical history when considering medication and other biologically focused interventions. Below is a compact comparison of core biological contributors and their clinical relevance.
Different biological contributors point to specific mechanisms and treatment considerations.
How Genetics and Family History Can Increase Depression Risk
Genetic factors raise susceptibility to MDD but do not determine outcome on their own. Heritability estimates show a moderate familial contribution; genes shape sensitivity to stress and interact with life experiences. [3] Research on variants affecting serotonin transport and stress-response pathways illustrates this gene–environment interplay rather than a single-gene cause.
Clinically, a family history of mood disorders increases the likelihood of recurrence and may prompt earlier intervention, more frequent monitoring during stressful periods, cautious medication selection, and consideration of higher-intensity services when multiple risks converge.
Brain Chemistry and Neurotransmitters in Depression
Neurotransmitters, serotonin, norepinephrine, and dopamine, help regulate mood, arousal, and reward. Variations in these systems can make depressive symptoms more likely or persistent, but the phrase “chemical imbalance” oversimplifies network-level and receptor changes. [4] Many antidepressant medications act on these neurotransmitter pathways to restore functional signaling and reduce symptoms.
Medication management is a central biological intervention when neurotransmitter-related mechanisms are prominent or symptoms are severe; the choice of agent is guided by symptom patterns, side-effect profiles, and prior responses. In practice, combining medication with psychotherapy often leads to more durable improvement than either approach alone.
What Psychological Causes Contribute to Major Depressive Disorder?

Psychological contributors include maladaptive thinking patterns, chronic negative focus, difficulties with emotion regulation, and personality traits that raise vulnerability to stress. [5] These processes shape how people interpret setbacks, sustain rumination, and withdraw socially, behaviors that keep low mood in place and impair problem-solving.
Psychological mechanisms interact with biological sensitivity and environmental stressors to precipitate and maintain episodes. The sections below describe key psychological drivers and the clinical approaches, such as cognitive and dialectical strategies, that target them.
Psychological mechanisms often explain how stressful experiences become ongoing depressive symptoms.
- Rumination and Negative Schemas: Repetitive negative thinking prolongs low mood and narrows perceived solutions.
- Learned Helplessness: Perceived lack of control increases inactivity and hopelessness.
- Personality Traits: High neuroticism or avoidant styles heighten stress sensitivity and interpersonal strain.
These psychological targets often guide therapy choices like CBT, DBT, and trauma-informed approaches that reshape thinking and bolster emotion regulation.
How Thinking Patterns and Emotional Health Affect Depression
Patterns such as rumination, cognitive distortions, and entrenched negative beliefs change how events are interpreted and can prolong depressive episodes by reinforcing hopeless thoughts and withdrawal. Difficulties regulating emotion, such as suppression or avoidance, reduce adaptive coping and increase physiological stress, which further entrenches symptoms.
Psychotherapies, including cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT), teach skills to break rumination, reframe unhelpful beliefs, and increase tolerance for difficult emotions. [6] Addressing these patterns lowers relapse risk and improves response to medication and structured outpatient programs.
How Stress and Personality Traits Can Increase Depression Risk
Yes. Ongoing stressors and certain personality features amplify biological vulnerabilities and raise both the likelihood of a first episode and the risk of recurrence. [7] Chronic HPA axis activation and maladaptive coping patterns make reactions to loss, conflict, or long-term adversity more intense.
People with high trait neuroticism or limited coping strategies are more likely to develop symptoms under stress. Clinically, stress-management training, skills-based therapies, and targeted work for personality-linked patterns can reduce severity and speed recovery. Assessing personality and stress profiles helps match treatment intensity, from outpatient therapy to more structured programs.
What Environmental Triggers and Life Events Lead to Major Depression?
Environmental and psychosocial triggers that commonly precipitate MDD include adverse childhood experiences, acute losses, chronic medical illness, social isolation, financial strain, and substance misuse. [8]
These events interact with biological and psychological vulnerabilities to trigger depressive episodes. Immediate life events can be proximal triggers, while long-term social determinants sustain risk and make recovery harder. The table below summarizes typical environmental triggers and their impacts on onset and course.
Environmental triggers change how the body responds to stress and shape long‑term vulnerability.
How Childhood Trauma and Adverse Experiences Affect Depression
Adverse childhood experiences (ACEs) increase lifetime risk for MDD by biologically embedding stress, altering HPA axis function, increasing inflammatory tendencies, and reshaping emotion-regulation networks. [9]
As a result, adults with trauma histories often present with more complex symptoms, higher rates of comorbid anxiety or substance use, and greater treatment resistance when trauma is unrecognized. [10] Trauma-informed therapies that address traumatic memory and teach regulation skills are central to effective care. Routine screening for ACEs and tailoring treatment to trauma histories improve engagement and outcomes.
Common Life Stressors and Social Factors That Can Trigger Depression
Common triggers include job loss, relationship breakdown, caregiving burden, serious illness, and social isolation, each of which disrupts resources and increases feelings of helplessness. Social determinants such as unstable housing, unemployment, and limited access to care compound risk and slow recovery.
Interventions that rebuild social support, connect people with community resources, and address practical needs work alongside clinical treatments to reduce relapse risk. Effective care plans routinely blend psychosocial supports with psychotherapy and medication when indicated.
How Do These Causes Inform Evidence-Based Treatment for Major Depressive Disorder?
Identifying the dominant causes in a person’s presentation helps clinicians choose evidence‑based treatments that match likely mechanisms. Biological drivers often lead to medication management; psychological drivers point to CBT, DBT, or trauma‑focused therapies; and environmental contributors call for social supports and integrated services.
Care intensity is matched to severity and complexity, ranging from routine outpatient therapy and medication follow‑up to structured programs (PHP, IOP) for more severe impairment. The short mapping below illustrates typical clinical pathways from cause to treatment.
Linking causes to treatment helps clinicians create personalized, mechanism‑focused plans.
- Neurotransmitter‑related symptoms → Medication management: Antidepressants and careful monitoring address mood and energy dysregulation.
- Cognitive/emotional drivers → Psychotherapy: CBT, DBT, and EMDR target thinking patterns, emotion regulation, and trauma consequences.
- Severe functional impairment → Higher‑intensity programs: PHP and IOP provide daily structure, group therapy, and multidisciplinary support.
How Understanding Causes Improves Therapy and Medication Choices
When clinicians identify whether biological, psychological, or social factors are most prominent, they can prioritize interventions with the strongest rationale, improving efficiency and outcomes.
For example, a clear trauma history supports early use of trauma-focused therapy like EMDR plus skills work, while marked anergia and psychomotor slowing may prompt medication optimization and medical evaluation.
Ongoing assessment lets teams adjust medications, shift therapeutic approaches, or escalate to PHP/IOP when response is only partial. Collaboration between prescribers and therapists ensures treatment addresses root drivers, not just surface symptoms.
Personalized Depression Treatment Options in Massachusetts
Adults in Massachusetts can access a broad range of evidence‑based outpatient services tailored to the cause and severity of MDD: Massachusetts medication management, individual psychotherapy, DBT, EMDR, trauma‑informed care, group therapy, and structured levels of care such as Partial Hospitalization Program (PHP), Intensive Outpatient Program (IOP), and standard Outpatient Program (OP).
Clinicians match intensity to need, PHP for marked functional impairment, IOP for persistent moderate symptoms, and OP for routine therapy and medication follow‑up.
For adults seeking discreet, hospitality‑oriented outpatient care with an experienced clinical team, Grand Rising Behavioral Health in Norwood, MA, offers personalized PHP, IOP, and OP pathways plus coordinated medication management; call (781) 604-1956 to discuss admissions and program fit.
For many people, combining medication, psychotherapy, and practical supports leads to better outcomes. Local programs emphasize integrated, individualized plans aligned with each person’s causal profile.
- Medication Management: Address biological mechanisms and monitor response.
- Psychotherapy (CBT/DBT/EMDR): Target thinking patterns, regulation, and trauma.
- Structured Programs (PHP/IOP/OP): Offer graduated intensity based on severity and function.
Frequently Asked Questions
What Are the Signs and Symptoms Of Major Depressive Disorder?
MDD commonly presents with persistent sadness or a flat mood, loss of interest or pleasure in activities, changes in appetite or weight, sleep disturbances, low energy, feelings of worthlessness or excessive guilt, and trouble concentrating.
Some people also report unexplained physical aches. Symptoms vary between individuals, and not everyone will have every symptom. Early recognition and professional help improve the chances of a good recovery.
How Is Major Depressive Disorder Diagnosed?
A qualified mental health professional makes the diagnosis using a clinical interview and standardized criteria such as those in the DSM-5. Clinicians assess symptom type, duration, and impact on daily function. Screening tools may be used to measure severity. A medical history and physical exam can help rule out medical conditions or medications that mimic depressive symptoms.
What Treatment Options Are Available for Major Depressive Disorder?
Treatment often combines psychotherapy, medication, and lifestyle strategies. Evidence-based therapies include Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), which address negative thinking and build emotion regulation skills.
Antidepressants, such as SSRIs or SNRIs, may be prescribed to help address neurotransmitter-related symptoms. Lifestyle changes like regular exercise, good sleep, and balanced nutrition support recovery and work best alongside professional care.
Can Lifestyle Changes Help Manage Major Depressive Disorder?
Yes. Regular physical activity, consistent sleep, a nutrient‑rich diet, and stress‑reduction practices (like mindfulness) can improve mood and support treatment. These changes are helpful but are most effective when paired with psychotherapy and/or medication when needed. Lifestyle adjustments are part of a comprehensive treatment plan, not a replacement for clinical care.
Disclaimer
The information in this article is meant for educational and informational purposes only. It should not replace professional medical or mental-health advice, diagnosis, or treatment. Grand Rising Behavioral Health offers evidence-based outpatient programs (including PHP, IOP, and OP), but individual needs and treatment timelines may vary.
If you or a loved one is dealing with mental health concerns, please reach out to Grand Rising Behavioral Health’s admissions team for a confidential consultation. Our licensed clinicians can evaluate your needs and help you start a safe, personalized care plan without delay.
Reference
1. https://www.nimh.nih.gov/health/publications/depression
2. https://www.who.int/news-room/fact-sheets/detail/depression
3. https://pmc.ncbi.nlm.nih.gov/articles/PMC3077049/
4. https://www.ncbi.nlm.nih.gov/books/NBK559078/
5. https://www.ncbi.nlm.nih.gov/books/NBK215119/
7. https://pmc.ncbi.nlm.nih.gov/articles/PMC3220767/
8. https://www.ncbi.nlm.nih.gov/books/NBK215119/
9. https://academic.oup.com/eurpub/article/35/5/896/8173708
10. https://www.ncbi.nlm.nih.gov/books/NBK207191/
More Resources
A team ready to start your journey.
Get in touch — today.
We are a safe space – a haven for exceptional individuals to receive discreet, personalized, in-person treatment and care.
.avif)










